June 1, 2020
Stroke is the fifth leading cause of death for Americans according to the CDC. In fact, strokes are responsible for one out of every 20 deaths. Is there a relationship between COVID-19 (or SARS-COV-2, the new coronavirus that causes it) and stroke? What can you do to help protect yourself from stroke, during the pandemic or anytime? What measures are hospitals taking to help ensure patients receive care quickly and safely?
Vascular neurologist Yazan Alderazi, MD, with UTHealth Neurosciences answers some of these pressing questions and offers tips for staying safe. Dr. Alderazi is affiliated with Memorial Hermann and is an assistant professor of neurology at McGovern Medical School at The University of Texas Health Science Center at Houston (UTHealth).
Is there a relationship between COVID-19 and stroke?
As Dr. Alderazi explains, “There are still a lot of uncertainties about the short- and longer-term effects of the coronavirus on the body, including on the brain and cardiovascular system. However, early data seem to suggest a relationship, at least an indirect relationship, between the virus and stroke, including in younger people.
“The belief is that SARS-COV-2 infects the respiratory system, then the body's immune system interacts with the virus. This response (activation and interaction of the immune system) is inflammation. The inflammation triggers the blood clotting system (coagulation system) in the body causing blood clots to form (thrombosis),” says Dr. Alderazi. “The blood clots (thrombi) then travel in the blood stream and get stuck in the arteries of the brain, causing a stroke. Other types of stroke have also been observed in COVID-19 patients, such as those due to blood clots forming in the veins that drain the brain.”
There has always been a connection between stroke and respiratory illnesses. “We've known for a long time that respiratory infections, like the flu and certain types of pneumonia, can increase the risk of stroke, especially in the first few days of contracting the infection. So it was not incredibly surprising to see that the coronavirus, which is primarily a respiratory illness, has caused, or seems to have caused, an increase in stroke incidents in some of the population studies,” says Dr. Alderazi.
“But I think what has taken people aback is the magnitude of how much stroke they're seeing, and, in particular, how young the patients are and how much blood-clotting is happening with the disorder,” he adds. “This needs further study to understand if this is out of proportion compared to other types of infection, but it does seem to be following that pattern.”
Don’t hesitate. Any stroke is a medical emergency. Seek immediate care.
A stroke occurs when a blood vessel supplying oxygen-rich blood to the brain is either blocked by a clot (ischemic stroke, representing 87% of strokes) or bursts (hemorrhagic stroke). “A stroke is always a medical emergency—during a pandemic or otherwise—and requires immediate medical care to avoid or minimize permanent damage,” says Dr. Alderazi.
A third type of stroke, a transient ischemic attack (TIA)—sometimes called a “mini-stroke,” blocks blood flow to the brain for temporarily—usually no more than 5 minutes. According to the American Heart Association/American Stroke Association, up to 25% of people who suffer a TIA die within one year, and about one-third of people who have a TIA go on to have a more severe stroke within one year.
“A TIA is also a medical emergency requiring emergency care, just like a major stroke, and is a warning sign of a future stroke. But initial data (following the outbreak of the new coronavirus) indicate that people experiencing minor strokes and people with stroke-like symptoms were not seeking medical care, perhaps for fear of becoming infected with (the virus that causes) COVID-19 in the hospital. Unfortunately, some waited until it became a major stroke, causing in some cases irreparable damage,” says Dr. Alderazi.
Patients should feel safe seeking emergency care for stroke or other health emergencies in any Memorial Hermann facility. Memorial Hermann has put additional safeguards in place to ensure the health and safety of all of its patients, its workforce and the community. Memorial Hermann’s Safe Wait™ is a new protocol that reinforces social distancing and other safety measures to make health care appointments and treatments as safe as possible.
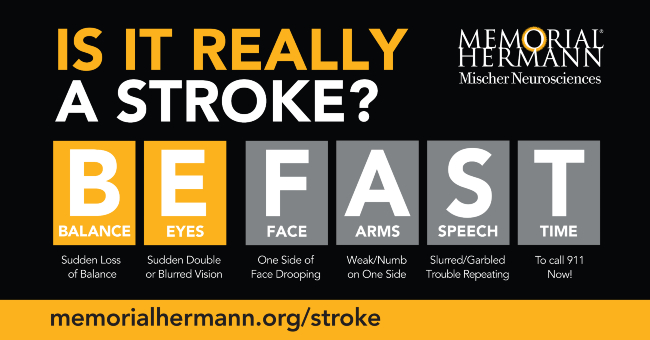
Know the warning signs of stroke. BE FAST. Call 911.
To spot a stroke, remember the acronym BE FAST:
If someone shows any of these symptoms, call 911 immediately.
Minimize your risk of stroke.
Certain populations are at a higher risk of stroke, including people with high blood pressure (hypertension) , people who smoke, people who are obese, people with diabetes, high cholesterol, heart disease and/or irregular heartbeat (atrial fibrillation) and people who are physically inactive. Not coincidentally, these individuals are also at a higher risk of developing complications from COVID-19.
“To protect yourself from stroke, don’t smoke. Know your numbers—your blood pressure, BMI (body mass index, an indicator of obesity) and cholesterol levels. Exercise at least 30 minutes a day. And if you’re overweight, commit to losing the weight,” says Dr. Alderazi.
Take extra precautions.
“While the threat of COVID-19 still exists, make sure you practice social distancing, wear a mask and wash your hands thoroughly and frequently. If you’ve had a stroke or are at higher risk of stroke, take extra precautions. Stay on top of your medications, including your blood pressure, cholesterol and diabetes medications. And stay in contact with your doctor—in clinic or via telemedicine,” says Dr. Alderazi.
Stay in touch.
“Even though they're physically distancing, stroke victims and their families and/or caretakers should stay in contact with each other. It’s especially important to check on people who live alone, because when a person has a stroke, they often need a family member or loved one to call 911. And as I’ve said earlier, when it comes to stroke, timing is critical,” says Dr. Alderazi.
Get a flu shot.
“The flu normally causes an increase in stroke (as well as heart attacks) in our population in the winter. It’s important that people get vaccinated against the flu, especially since we're going to be headed into the flu season this year not knowing if it's going to be a flu plus coronavirus season. Unlike the flu virus, the flu vaccine does not increase a person’s risk of stroke. Whatever we can do to keep people healthy is important,” says Dr. Alderazi.
Trust Memorial Hermann for stroke care. “If you or a loved one is experiencing stroke symptoms, don’t wait. It's extremely important that people continue to seek care for these emergencies and trust that we will keep them safe to the best of our abilities. We are prepared,” says. Dr. Alderazi.
To learn more about the warning signs of stroke or stroke care at Memorial Hermann, click here. To schedule an appointment with a neurologist affiliated with Memorial Hermann, visit memorialhermann.org/doctors or call (713) 704-7100.